The term telemedicine refers to utilization of telecommunication technology for medical diagnosis, treatment, and patient care. Telemedicine enables a physician or specialist at one site to deliver health care, diagnose patient, give intra-operative assistance, provide theraphy or consult with another physician or paramedical personel at remote site.
The aim of telemedicine is to provide expert-based health care to understaffed remote sites and to provide advanced emergency care through modern telecommunication and information technologies.
This tabel below is result from survey did by WHO for Indonesia.
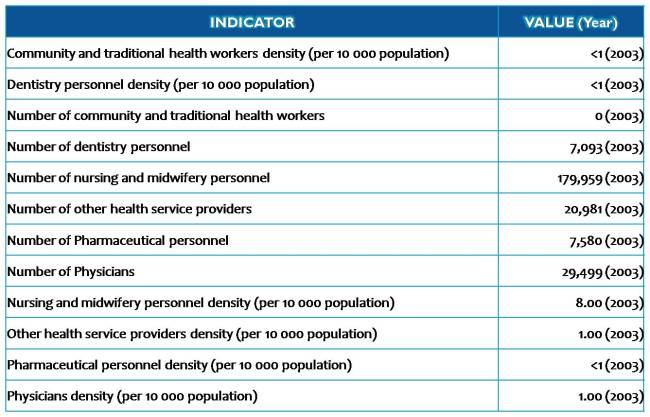
core health indicator (Indonesia) by WHOSIS
In general, Indonesia only has one physician per 10 000 population. Countries with fewer than 25 health care professionals (counting only physicians, nurses and midwives) per 10 000 population failed to achieve adequate coverage rates for selected primary health care interventions as prioritized by the Millennium Development Goals framework (WHO 2006).
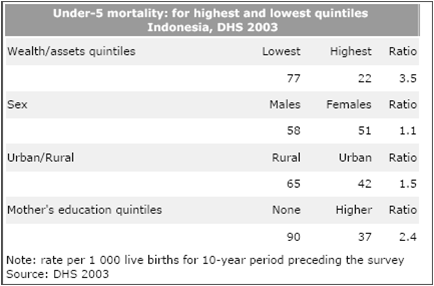
From table above, we can see that in rural area, there is more death for under-five children than in urban area. Rural area needs more physician so the people can take care of their health. Can the government provide these physicians?
Telemedicine is a nice solution. The government can equip the health care facilities on rural areas (e.g. Puskesmas) with telemedicine system that connect with main hospital at province capital. They also need create new health system that support this telemedicine system, like diagnose system, pharmaceutical system, post-hospital monitoring system, home-care monitoring system, etc.
In May 1999 a joint trial project in Telemedicine was launched by MEDIFA, an Indonesian NPO that supports the training of young doctors, and the Japan International Co-operation Agency (JICA), advisors to the Indonesian Government on telecommunications policy. The project uses low price videophone equipment to enable local doctors to consult specialists in major hospitals through conventional telephone lines. Based on the results of the trial, MEDIFA expanded the network of videophones to 80 clinics.
The trial aimed to find a practical and inexpensive way for local doctors in outlying regions to consult medical specialists and take part in medical education. This provided a better service for patients, while helping to train the doctors.
(1) Necessity
Doctors in regional clinics sometimes lack experience in certain fields and are hesitant in their diagnoses without the back-up of senior doctors at major hospitals. Both local doctors and patients want to be able to consult specialists in difficult cases “face-to-face” via videophones.
(2) System Requirements
- Face-to-face communications
- Nationwide access to the network possible
- Ease of use
- Low cost for sustainable operation (including equipment and telephone charge).
(3) Advantages of using videophones via conventional phone lines:
- Applicable in any area with a telephone network
- Easy to use (Personal computer not required)
- Economical: US $450 for equipment + telephone charges.*
*(Videophones using ISDN networks provide better quality images, but the ISDN service is available only in limited areas and the equipment would cost more than US $4,000 per site.)
The trial project was implemented at five clinics within 100 km of Jakarta, linking them with the Chipto Mangunkusmo hospital in Jakarta.
Implementation of trial project :
- In May 1999, JICA experts provided videophones and TV sets, and “MEDIFA” started the trial.
- From May to the beginning of June 1999, phase 1 of the Telemedicine trial was implemented, with no charge made for consulting specialists at the central hospital.
- From the middle of June to the middle of October 1999, phase 2 was implemented, this time with a charge being made for consulting specialists.
- In March 2000, MEDIFA expanded the Telemedicine network to 80 clinics, using small-scale grant aid from the Japanese Embassy in Indonesia.
Configuration and equipment :




The project showed that Telemedicine can be effective, as well as sustainable without operational subsidies from government.
The introduction of Telemedicine using a low cost videophone system is expected to not only enable patients to consult specialists that they might not otherwise have access to; it is also expected to help improve the abilities of young, local doctors in provincial and rural areas.
The picture quality equalled VHS video quality for still pictures. Even imperfect moving pictures contribute to better communication between doctors and enable local doctors to get advice from senior colleagues by showing a patient’s symptoms and condition.
 Specifications of videophone (TV400):
Specifications of videophone (TV400):
Picture: NTSC/PAL
Camera: 1/4″ CCD
CIF 352 x 288 pic-cell
QCIF 176 x 144 pic-cell
SQCIF 128 x 96 pic-cell
Max. 15 frames/sec.
Modem speed: Max. 33.6kbps
Interface: ITU-T H.324 (System)
H.263 (Video)
G.723 (Audio)
Power: 90~260V, 50/60Hz, 12W
Size: 60 (H) x 140 x 180 (D) mm
Providing medical consultations via videophone is effective, sustainable and ready for actual operation, especially in the specialities of internal medicine and dermatology.
In order to improve its effectiveness, the system should be centred, if possible, on a 24-hour emergency department of a major hospital.
Tele-education to help train local doctors is also effective, especially in the fields of internal medicine and dermatology.
Using a small-scale grant aid from Japanese embassy in Indonesia, MEDIFA expanded the videophone network to 80 clinics, together with the establishment of an online library of Tele-education seminars and medical information.